Reproducibility in Temperature Measurement
Multiple temperature readings in the same area, mouth, rectum, axilla, ear or temporal artery, make for variability with each separate measurement. This can be confusing for clinicians, since they expect the same number with each measurement. The
Oral Temperature
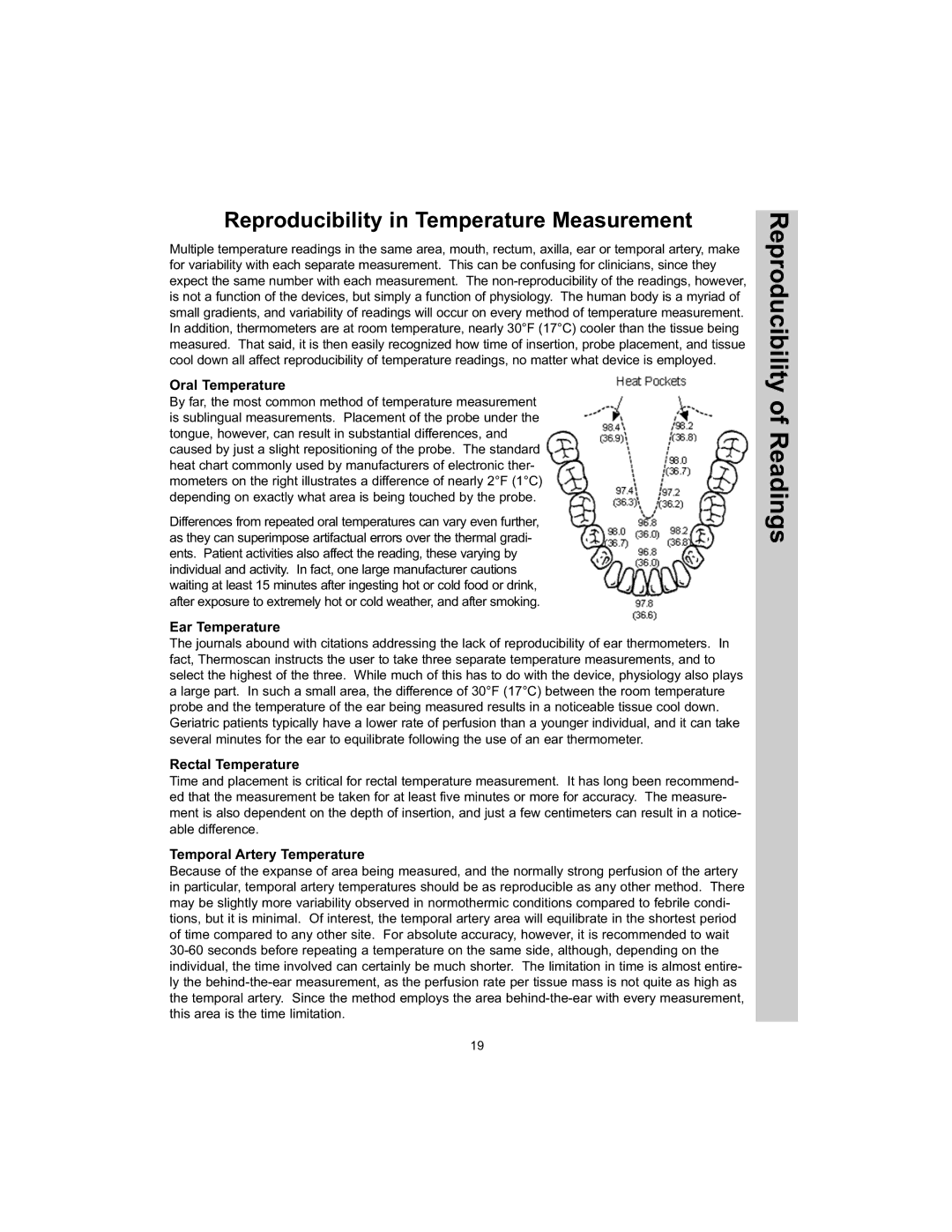
By far, the most common method of temperature measurement is sublingual measurements. Placement of the probe under the tongue, however, can result in substantial differences, and caused by just a slight repositioning of the probe. The standard heat chart commonly used by manufacturers of electronic ther- mometers on the right illustrates a difference of nearly 2°F (1°C) depending on exactly what area is being touched by the probe.
Differences from repeated oral temperatures can vary even further, as they can superimpose artifactual errors over the thermal gradi- ents. Patient activities also affect the reading, these varying by individual and activity. In fact, one large manufacturer cautions waiting at least 15 minutes after ingesting hot or cold food or drink, after exposure to extremely hot or cold weather, and after smoking.
Ear Temperature
The journals abound with citations addressing the lack of reproducibility of ear thermometers. In fact, Thermoscan instructs the user to take three separate temperature measurements, and to select the highest of the three. While much of this has to do with the device, physiology also plays a large part. In such a small area, the difference of 30°F (17°C) between the room temperature probe and the temperature of the ear being measured results in a noticeable tissue cool down. Geriatric patients typically have a lower rate of perfusion than a younger individual, and it can take several minutes for the ear to equilibrate following the use of an ear thermometer.
Rectal Temperature
Time and placement is critical for rectal temperature measurement. It has long been recommend- ed that the measurement be taken for at least five minutes or more for accuracy. The measure- ment is also dependent on the depth of insertion, and just a few centimeters can result in a notice- able difference.
Temporal Artery Temperature
Because of the expanse of area being measured, and the normally strong perfusion of the artery in particular, temporal artery temperatures should be as reproducible as any other method. There may be slightly more variability observed in normothermic conditions compared to febrile condi- tions, but it is minimal. Of interest, the temporal artery area will equilibrate in the shortest period of time compared to any other site. For absolute accuracy, however, it is recommended to wait
Reproducibility of Readings
19