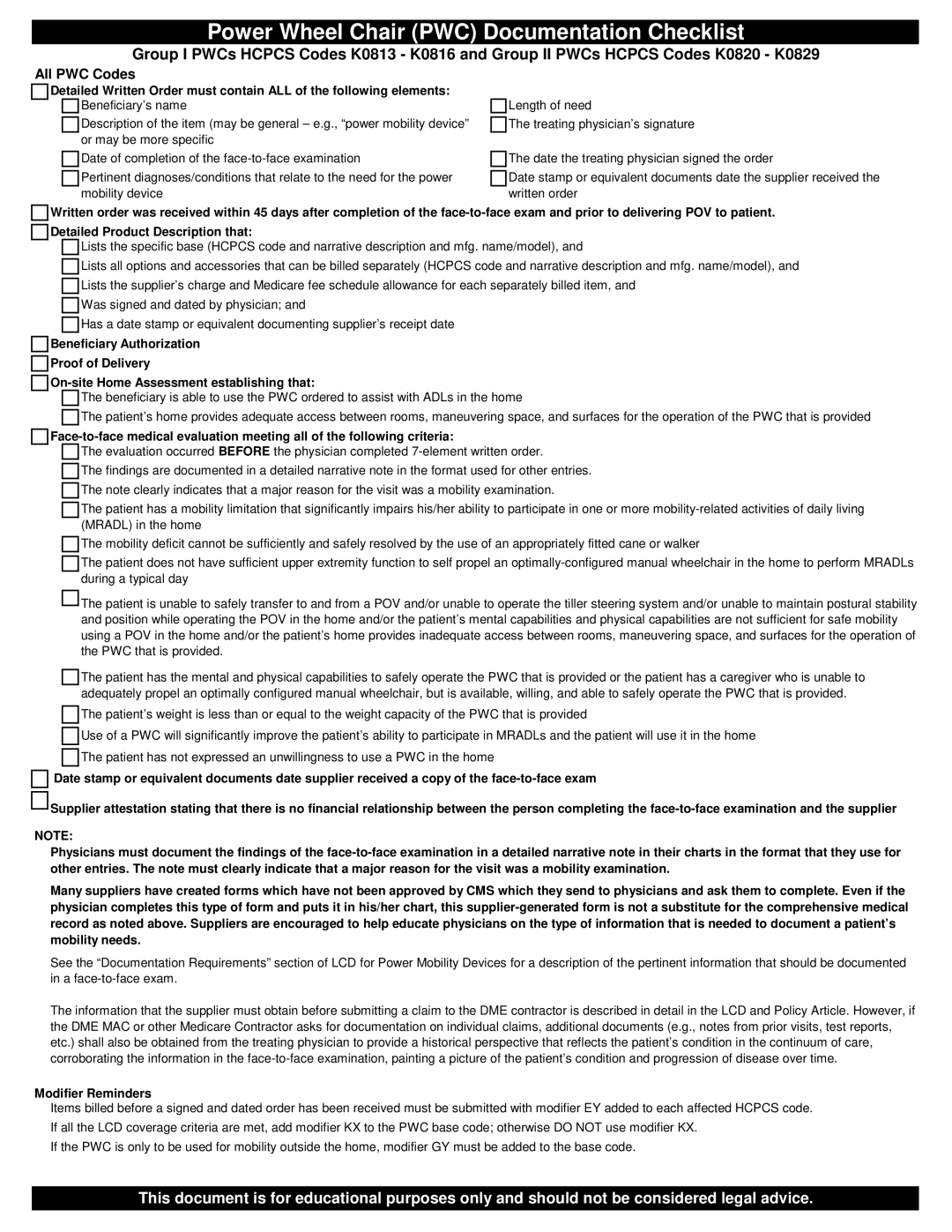
Power Wheel Chair (PWC) Documentation Checklist
Group I PWCs HCPCS Codes K0813 - K0816 and Group II PWCs HCPCS Codes K0820 - K0829
All PWC Codes
Detailed Written Order must contain ALL of the following elements:
Beneficiary’s name
Description of the item (may be general – e.g., “power mobility device” or may be more specific
Length of need
The treating physician’s signature
Date of completion of the
Pertinent diagnoses/conditions that relate to the need for the power mobility device
The date the treating physician signed the order
Date stamp or equivalent documents date the supplier received the written order
Written order was received within 45 days after completion of the
Detailed Product Description that:
Lists the specific base (HCPCS code and narrative description and mfg. name/model), and
Lists all options and accessories that can be billed separately (HCPCS code and narrative description and mfg. name/model), and
Lists the supplier’s charge and Medicare fee schedule allowance for each separately billed item, and
Was signed and dated by physician; and
Has a date stamp or equivalent documenting supplier’s receipt date
Beneficiary Authorization
Proof of Delivery
The beneficiary is able to use the PWC ordered to assist with ADLs in the home
The patient’s home provides adequate access between rooms, maneuvering space, and surfaces for the operation of the PWC that is provided
The evaluation occurred BEFORE the physician completed
The findings are documented in a detailed narrative note in the format used for other entries.
The note clearly indicates that a major reason for the visit was a mobility examination.
The patient has a mobility limitation that significantly impairs his/her ability to participate in one or more
The mobility deficit cannot be sufficiently and safely resolved by the use of an appropriately fitted cane or walker
The patient does not have sufficient upper extremity function to self propel an
![]()
![]() The patient is unable to safely transfer to and from a POV and/or unable to operate the tiller steering system and/or unable to maintain postural stability
The patient is unable to safely transfer to and from a POV and/or unable to operate the tiller steering system and/or unable to maintain postural stability
and position while operating the POV in the home and/or the patient’s mental capabilities and physical capabilities are not sufficient for safe mobility using a POV in the home and/or the patient’s home provides inadequate access between rooms, maneuvering space, and surfaces for the operation of the PWC that is provided.
The patient has the mental and physical capabilities to safely operate the PWC that is provided or the patient has a caregiver who is unable to adequately propel an optimally configured manual wheelchair, but is available, willing, and able to safely operate the PWC that is provided.
The patient’s weight is less than or equal to the weight capacity of the PWC that is provided
Use of a PWC will significantly improve the patient’s ability to participate in MRADLs and the patient will use it in the home
The patient has not expressed an unwillingness to use a PWC in the home
Date stamp or equivalent documents date supplier received a copy of the
![]()
![]() Supplier attestation stating that there is no financial relationship between the person completing the
Supplier attestation stating that there is no financial relationship between the person completing the
NOTE:
Physicians must document the findings of the
Many suppliers have created forms which have not been approved by CMS which they send to physicians and ask them to complete. Even if the physician completes this type of form and puts it in his/her chart, this
See the “Documentation Requirements” section of LCD for Power Mobility Devices for a description of the pertinent information that should be documented in a
The information that the supplier must obtain before submitting a claim to the DME contractor is described in detail in the LCD and Policy Article. However, if the DME MAC or other Medicare Contractor asks for documentation on individual claims, additional documents (e.g., notes from prior visits, test reports, etc.) shall also be obtained from the treating physician to provide a historical perspective that reflects the patient’s condition in the continuum of care, corroborating the information in the
Modifier Reminders
Items billed before a signed and dated order has been received must be submitted with modifier EY added to each affected HCPCS code.
If all the LCD coverage criteria are met, add modifier KX to the PWC base code; otherwise DO NOT use modifier KX.
If the PWC is only to be used for mobility outside the home, modifier GY must be added to the base code.
This document is for educational purposes only and should not be considered legal advice.