Invacare® Therapeutic Support Surfaces
Therapeutic Support Surfaces
Therapeutic Support Surfaces prevent and treat pressure ulcers by molding to the body to maximize contact, redistributing weight as uniformly as possible, and reducing pressure to below capillary closure (32mm/Hg).3 While a variety of support surfaces have been shown to improve pressure ulcers, there is no compelling evidence that
one support surface consistently performs better than all others, under all circumstances. The primary concern when choosing a support surface should be the therapeutic benefit associated with the product.
Invacare’s TSS line consists of Group I and Group II surfaces as defined by CMS. Each Group can further be categorized by the type of surface and whether it is dynamic or static.
Group I - Support surfaces designed to prevent pressure ulcers
•Gel Overlay – Uniformly distributes pressure and reduces friction and shear with gel bladders inside a foam core. Designed to be placed directly on top of an existing mattress.
•Foam Mattress – Multiple layers of foam for maximum pressure reduction. Designed to be placed directly on the existing bed frame.
•Alternating Pressure Pad – Alternates inflation and deflation of cells to constantly change pressure points. Designed to be placed directly on top of an existing mattress.
Group II - Support surfaces designed to prevent and treat pressure ulcers
•Non Powered Pressure Reducing Mattress – Channels air through cells for maximum patient immersion.
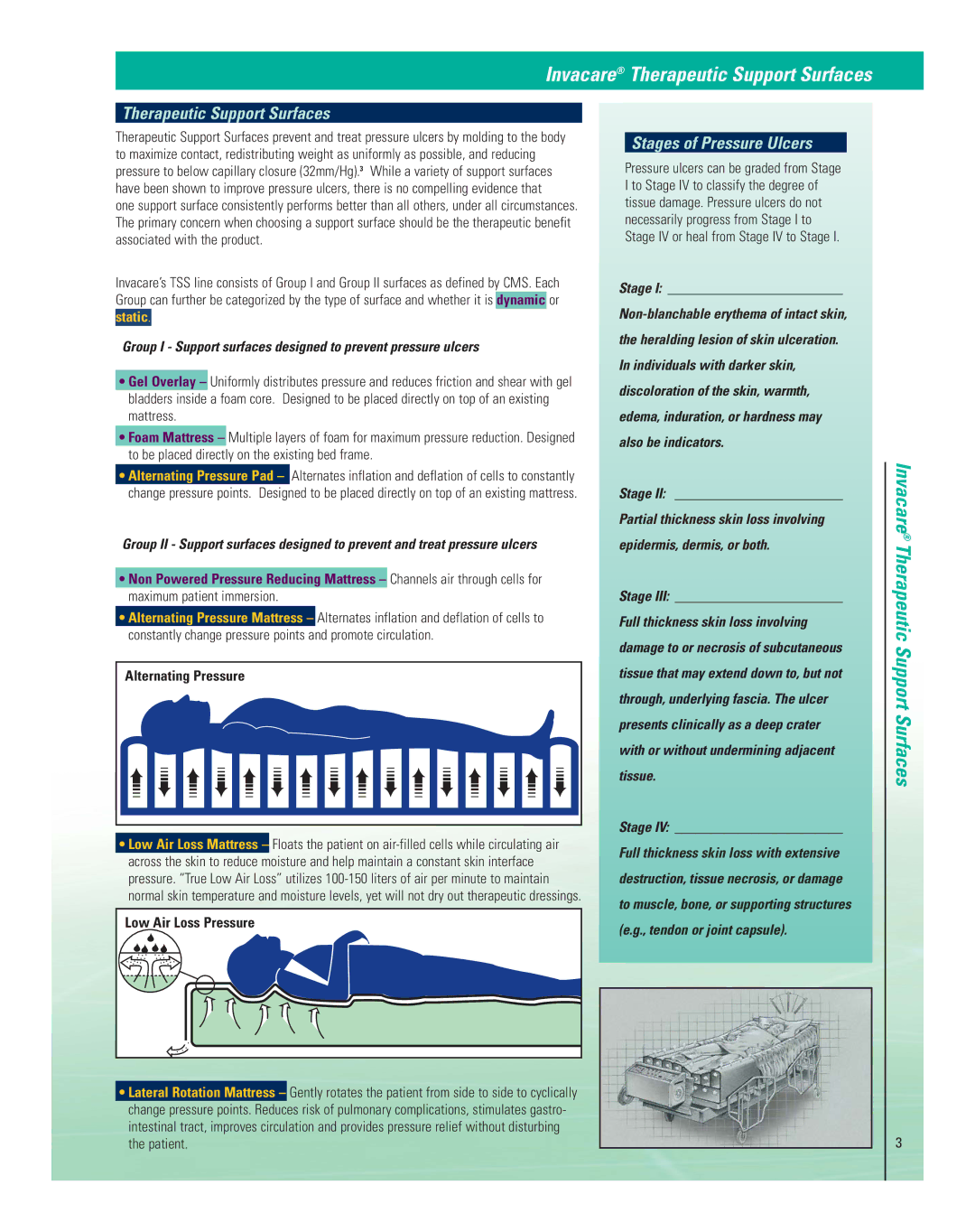
•Alternating Pressure Mattress – Alternates inflation and deflation of cells to constantly change pressure points and promote circulation.
Alternating Pressure
•Low Air Loss Mattress – Floats the patient on
Low Air Loss Pressure |
•Lateral Rotation Mattress – Gently rotates the patient from side to side to cyclically change pressure points. Reduces risk of pulmonary complications, stimulates gastro- intestinal tract, improves circulation and provides pressure relief without disturbing the patient.
Stages of Pressure Ulcers
Pressure ulcers can be graded from Stage
I to Stage IV to classify the degree of tissue damage. Pressure ulcers do not
necessarily progress from Stage I to
Stage IV or heal from Stage IV to Stage I.
Stage I: _________________________
the heralding lesion of skin ulceration.
In individuals with darker skin,
discoloration of the skin, warmth,
edema, induration, or hardness may
also be indicators.
Stage II: ________________________
Partial thickness skin loss involving
epidermis, dermis, or both.
Stage III: ________________________
Full thickness skin loss involving
damage to or necrosis of subcutaneous
tissue that may extend down to, but not
through, underlying fascia. The ulcer
presents clinically as a deep crater
with or without undermining adjacent
tissue.
Stage IV: ________________________
Full thickness skin loss with extensive
destruction, tissue necrosis, or damage
to muscle, bone, or supporting structures
(e.g., tendon or joint capsule).
Invacare® Therapeutic Support Surfaces
3